People with poor bowel habits also have poor sleep quality
We cite and refer to a research paper entitled 東京圏の成人女性を対象とした便通状態と睡眠健康に関する疫学的調査.
Patients with abnormal bowel movements are more drowsy and sleep less than those in the good bowel movement group. They also have irregular bedtimes, sleeping hours, and sleep habits related to their biological rhythms.
Gastrointestinal tract activity
Gastrointestinal motility has a similar sleep-wake rhythm, being active when awake and calm when asleep. And muramyl peptides derived from the cell walls of intestinal bacteria in the colon act as sleep substances. It is also known that the growth state of intestinal bacteria is influenced by the state of gastrointestinal motility. Therefore, the state of motility of the large intestine, the home of the intestinal bacteria, or bowel movements, may affect sleep.
Types of Gastrointestinal Diseases
Irritable bowel syndrome (IBS) and functional constipation (FC) are the most common digestive disorders. Irritable bowel syndrome (IBS) is a disorder characterized by abdominal pain, diarrhea, mucous stools, constipation, and bloating due to increased intestinal motility and hypersecretion caused by persistent parasympathetic nervous system tension. On the other hand, functional constipation (FC) is a type of constipation in which stools remain in the colon for a long time and become hard due to excessive water absorption, because the intestinal tensions are loosened and intestinal motility is not performed. This type of constipation is more common in women. Irritable bowel syndrome (IBS) is significantly more common in young women, with an estimated incidence of about 25% in Japan. Irritable bowel syndrome (IBS) patients have found that poor sleep quality the night before correlates with worse irritable bowel syndrome (IBS) the next day, and that irritable bowel syndrome (IBS) increases REM sleep (shallow sleep). It can be assumed that the quality of life of irritable bowel syndrome (IBS) patients is impaired and under tremendous stress.
Method of investigation
Female daily workers, female students and housewives aged 20-45 living in the Tokyo area were randomly selected. The number of data used for the analysis was 988. Because seasonal changes in sunlight hours, temperature, and other factors strongly affect sleep health, a questionnaire was used to survey sleep status during May in the first week of June. The questions regarding sleep health were as follows, consisting of categorized and uncategorized items.
- Categorized items
- Factor 1: Factors related to sleep maintenance disorder
- Number of awakenings in the middle of the day
- Feeling of sound sleep
- Nocturnal urination frequency
- Early-morning alertness
- Factor 2: Factors related to sleep parasomnias (parasomnias, sleepwalking behavior during sleep)
- Degree of sleepiness occurrence
- Degree of sleep paralysis occurrence
- Degree of occurrence of hallucinations during fearful sleep onset
- Degree of occurrence of abnormalities in restless legs and limb movements
- Factor 3: Sleep apnea-related factors
- Degree of snoring occurrence
- Degree of sleep apnea occurrence
- Factor 4: Factors related to difficulty in getting up
- Difficulty getting up
- Time to floor release
- Factor 5: Factors related to sleep onset disorders
- Frequency of sleeping pill use
- Sleep latency (the time it takes to fall asleep)
- Factor 1: Factors related to sleep maintenance disorder
- Uncategorized items
- Bedtime
- Wake-up time
- Irregularity of bedtime
- Irregularity of wakingtime
- hours of sleep
- Irregularity in sleeping hours
- Sleep deprivation
- Weekday sleepiness
For questions related to frequency, such as the number of awakenings and nocturnal urination, participants were asked to fill in the number of times, for questions related to time away from the bed and latency to fall asleep (the time it takes to fall asleep), and for questions related to time of day, such as time of going to bed and time of waking, participants were asked to fill in the time. For the other questions, participants were asked to choose one of four levels of sleep (only the feeling of sound sleep was given a five-level scale). The respondents were also asked about their eating habits and their exercise habits (at least 30 minutes per day) as lifestyle habits that may affect sleep health.
Results of a survey
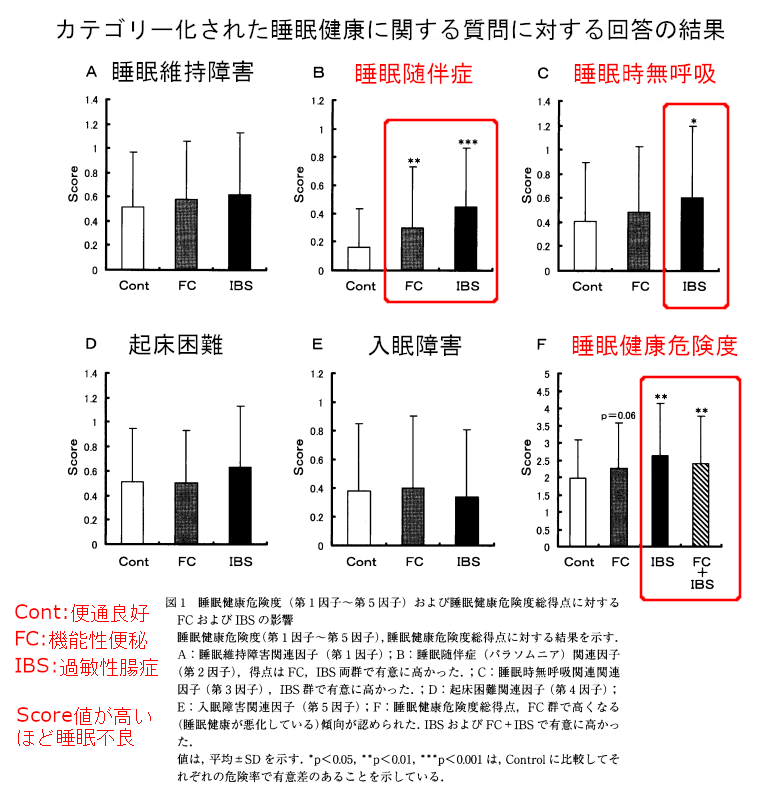
The figure above shows the responses to the categorical questions. The results show that people with irritable bowel syndrome (IBS) or functional constipation (FC) have higher Score values on factors related to sleep parasomnias and sleep apnea than those with good bowel movements (Cont), indicating that they sleep poorly.The F Sleep Health Risk Score is an overall rating from A to E. People with irritable bowel syndrome (IBS) and irritable bowel syndrome (IBS)+functional constipation (FC) still have higher Score values.
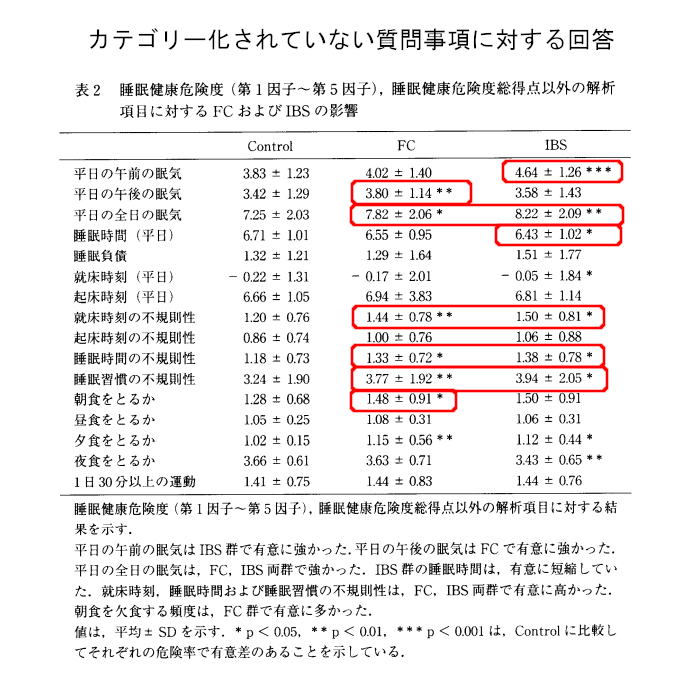
The figure above shows the answers to the uncategorized questions.
Weekday morning sleepiness was higher in irritable bowel syndrome (IBS) than in good bowel movement group (Control), weekday afternoon sleepiness was higher in functional constipation (FC) than in good bowel movement group (Control). The sleepiness on the day before the weekday was higher in the irritable bowel syndrome (IBS) and functional constipation (FC) groups than in the control group. This means that people with poor bowel movements are more likely to feel sleepy.
Irregularity in bedtime, sleep duration, and sleep habits is higher in both irritable bowel syndrome (IBS) and functional constipation (FC) than in the good bowel movement group (Control). People with poor bowel movements are more irregular in terms of sleep other than waking time.
The frequency of skipping breakfast increased functional constipation (FC) compared to the control group. The frequency of skipping dinner increased both in irritable bowel syndrome (IBS) and functional constipation (FC) compared to the control group. Does this mean that people with functional constipation (FC) eat less often? If you don’t eat, you can’t have a bowel movement, right?
There was no difference with respect to locomotion.
As sleep worsens, quality of life declines, and the decline becomes more pronounced as the degree of insomnia increases. Insomnia also decreases physical and mental activity. They are 10 times more likely to miss work than those with good sleep health. Sleep is critical for a healthy and active social life.
Compared to the group with good bowel movements, the group with poor bowel movements had higher Score values for factors related to sleep parasomnias (parasomnias, sleepwalking behavior during sleep) and sleep apnea, resulting in poor sleep. Sleep parasomnias include sleepwalking, sleep paralysis, and fearful sleep hallucinations, which are reported to be increased by high levels of psychological stress, and the appearance of such sleep parasomnias tends to decrease the quality of sleep. The decreased quality of sleep at night in the irritable bowel syndrome (IBS) and functional constipation (FC) groups is likely to decrease daytime arousal levels the next day, and experimental results showed increased daytime sleepiness in the irritable bowel syndrome (IBS) and functional constipation (FC) groups. Furthermore, irritable bowel syndrome (IBS) patients had significantly less sleep on weekdays, and irritable bowel syndrome (IBS) patients with more severe bowel movement disorders may have insufficient sleep quantity as well as sleep quality.
How to improve bowel movements
Bowel movements should be improved in order to get a good night’s sleep, and the best way to improve them is to lead a regular life. First, set a wake-up time and get up in the morning sun. This will reset your body clock. Then, by regularly consuming food, the metabolic rhythms present in the liver and other organs can be governed. People have an inherent desire to defecate in the morning. This is due to the gastric-colon (the main part of the large intestine) reflex, which is strongest when there is no food in the stomach, i.e., when food enters the stomach in the morning after a good night’s sleep. Your mouth and anus are a distance apart, yet when you have breakfast, you may feel the urge to have a bowel movement, as if you are being pushed out. The high rate of skipping breakfast in the irritable bowel syndrome (IBS) and functional constipation group (FC) indicates that the regular gastro-colonic reflex is not occurring and the metabolic rhythm is disrupted.
Related Articles
It’s not just your metabolic rhythms that are disrupted, but your life in general.
Because the regular gastro-colonic reflex is not occurring, not only are metabolic rhythms disturbed, but biological rhythms in general may be disrupted. This is because the functional constipation group (FC) had a high degree of irregularity in bedtime, sleep duration, and sleep habits. And irritable bowel syndrome (IBS) had significantly regressed weekday bedtimes, and significantly higher irregular bedtimes, irregular sleep times, and even irregular sleep habits. And as sleep quality and quantity deteriorate, daytime arousal levels are lower. Quality of life will also be lower because you will not be able to do good work or concentrate highly while feeling sleepy. Sleep apnea-related factors were worse in irritable bowel syndrome (IBS) than in controls. In general, young women snore less frequently, which is a cause of sleep apnea. Snoring is mostly caused by increased upper airway resistance or by rhinitis or abnormal nasal septum, and occurs during light to moderate depth sleep. Exacerbation of sleep apnea-related factors in irritable bowel syndrome (IBS) may be due to shallow sleep with stress. And while obstruction, the main cause of obstructive sleep apnea, is thought to be due to muscle relaxation and tongue root subsidence, in irritable bowel syndrome (IBS) the peripheral gastrointestinal motor state may be affecting the brain’s respiratory center. The respiratory center is located in the medulla oblongata, and a group of nerves modifying the respiratory center is located in the bridge (part of the brainstem), where the respiratory rhythm is thought to be regulated. In addition, in humans, balloon dilation of the colon increases blood flow to the bridge and activates neural activity. This is thought to indicate that the state of peripheral gastrointestinal motility is constantly monitored by the brain and affects cranial nerve functions, including the respiratory center. In other words, the state of bowel movements (the state of gastrointestinal motility) makes sleep worse.



コメント