I don’t recommend drinking alcohol just because you can’t sleep.
The research paper アルコール依存症に関連する睡眠障害 is cited and referred to in this report.
When you become a working adult, you can drink alcohol, but you also experience a lot of stress. Not a few people find it difficult to sleep due to such stress. Also, unlike students, they have fewer opportunities to be physically active. And once a child is born, they have even less time for themselves and even less time for exercise. Then there are those who drink alcohol because they can’t sleep. Actually, I am one of those people. I have always been a drinker, so I drink almost every day. I can sleep because I feel sleepy as soon as I drink, but sometimes I wake up in the middle of the night. It would be fine if I could go to sleep immediately afterwards, but when I cannot sleep, I resort to drinking. And the next day, I have a hangover. During work, I lose concentration due to sleepiness. I have to distract myself from the frustration of a job that didn’t go well by drinking… This is the worst kind of routine.
Alcohol and Sleeping Pills
Drinking alcohol brings on drowsiness because alcohol has a depressant effect on the central nervous system. Drinking in moderation promotes falling asleep and increases the feeling of sound sleep. For this reason, alcohol has been used as a substitute for sleeping pills. Some people may think that alcohol is safe because it is easily available and found in food, while sleeping pills are considered dangerous. However, the alcohol used to relieve insomnia may be the cause of insomnia. Especially when alcoholism develops, the withdrawal period (when the substance, in this case alcohol, is removed from the body) can be accompanied by significant insomnia and even psychosomatic symptoms. This leads to a vicious cycle of increased alcohol consumption and further alcohol dependence. Some people tolerate alcohol intake during withdrawal and are able to continue to abstain from alcohol afterwards, but suffer from insomnia for many years. In addition, regular drinking can lead to problems such as sleep apnea and abnormal sleep behavior. Therefore, sleeping pills are safer than alcohol.
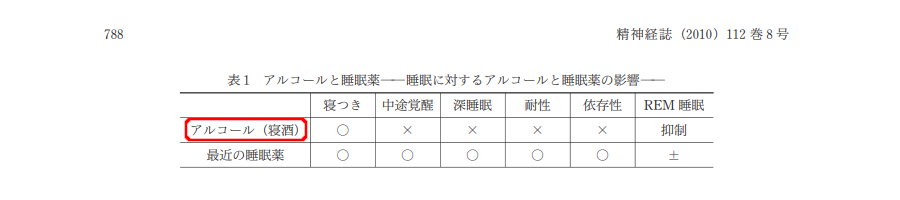
What makes alcohol excellent is that it helps you sleep better, tastes good, is fun, and you feel the love of its creator. Using it as a substitute for sleeping pills is dangerous. Benzodiazepines should be used with caution because of their effects on respiratory depression, muscle relaxation, and increased arousal range, but alcohol is also dangerous because it increases sleep apnea and abnormal sleep behaviors such as bouts of sleep apnea, sleepwalking, sleep talking, and teeth grinding.
What happens if alcohol is consumed before bedtime
If we drink around 1g of alcohol per kg of body weight before bed (about 1200ml of canned beer for a 60kg person) and investigate the effects of alcohol on nighttime sleep, we find the following changes. (1) Sleep time tends to decrease. This is because arousal increases in the latter half of sleep. (2) Sleep quality, REM sleep (shallow sleep in which information, emotions, and memories are considered to be organized) decreases in the first half of the night, but may increase compensatory in the second half. It decreases throughout the night with increasing amounts of alcohol, because alcohol has an inhibitory effect on REM sleep. However, after a week of continuous alcohol consumption, the REM sleep suppression effect diminishes. It increases counteractively when alcohol consumption is discontinued. There are many reports of a dose-dependent increase in slow wave sleep (the deepest sleep found in the first half of sleep).
What are Sleep Disorders During Alcohol Withdrawal?
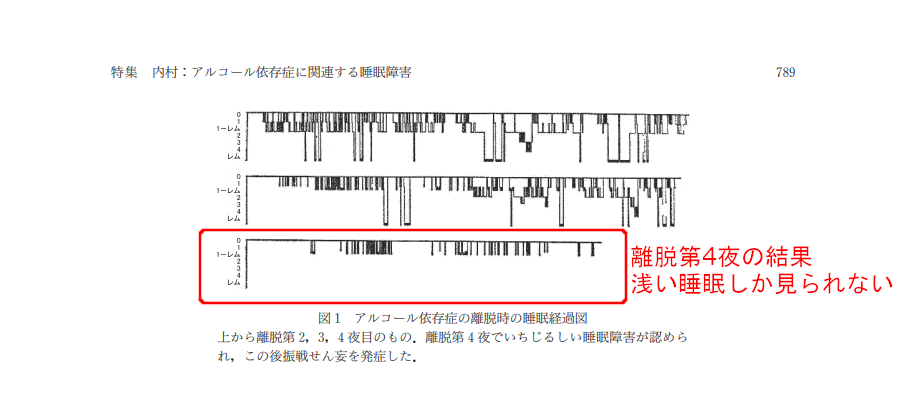
When alcoholics stop drinking, they often suffer from difficulty falling asleep and hypervigilance immediately afterwards. If the patient develops delirium tremens (so-called withdrawal symptoms), severe or sometimes complete insomnia with autonomic nervous system symptoms such as sweating and psychiatric symptoms, mainly impaired consciousness and hallucinations, may follow. Delirium tremens often lasts two to three days (rarely more than a week) and may end with a long, deep sleep (terminal sleep).
Polysomnographic studies of nocturnal sleep during and after delirium tremens have reported increased mid-waking, increased sleep stage shifts and shallower sleep, increased REM sleep, increased sleep stage 1 (the shallowest stage of non-REM sleep, which is deeper sleep than REM sleep), decreased slow wave sleep, longer onset latency (meaning it took longer to fall asleep) and shorter sleep duration.
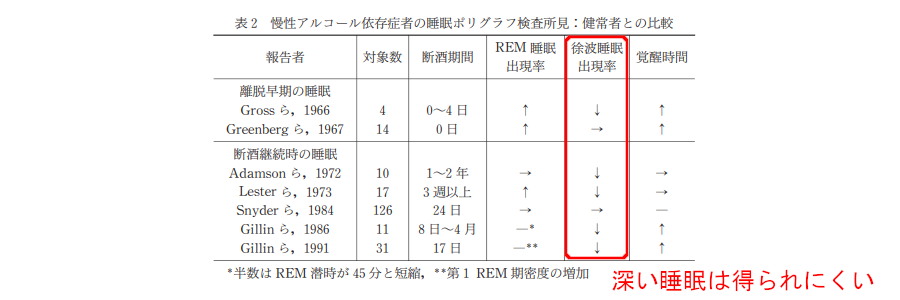
In addition, nocturnal sleep immediately after withdrawal and terminal sleep at the end of delirium tremens were recorded. The results showed that nocturnal sleep immediately after withdrawal increased in most cases to mid-wake and stage 1, and slow-wave sleep was significantly reduced or eliminated.
In Sleep in Continuing Alcoholics Anonymous
It has been observed that sleep fragmentation in alcoholics after 1 to 2 weeks of sobriety is progressively reduced compared to immediately after sobriety, and subjective sleep sensation also improves. However, some may continue to complain of anxiety, self-dependence, autonomic symptoms, and depressive symptoms for one to two months or even longer. This may be the cause of their relapsing into alcoholism. The incidence of slow-wave sleep has decreased over the years even during ongoing sobriety, and the decrease in slow-wave sleep may be irreversible. However, a person may have decreased slow-wave sleep but not complain of insomnia. There are also results showing phase advancement of circadian rhythms, such as a shortening trend in REM sleep latency until 3 months after sobriety and the predominant appearance of REM sleep in the first half of the day.
Treatment of Sleep Disorders Associated with Alcoholism
For alcoholics, relatively high doses (10-20 mg) of diazepam, which is cross-tolerant to alcohol and has anticonvulsant effects, are administered with adequate physical control for dehydration, etc., and then tapered off after 4-5 days. If delirium tremens appears, newer antipsychotics such as risperidone and quetiapine are effective. High doses (90-240 mg) of the antidepressant mianserin have been administered and found to be effective in treating withdrawal delirium and preventing its occurrence. Mianserin is considered effective as a withdrawal drug for alcoholics because of the high rate of depression in alcoholics, which may be a cause of insomnia and relapse to drinking, and because it is hypnotic but is not easily tolerated. Insomnia observed during post-withdrawal drinking should be treated in accordance with the usual treatment for insomnia, but care must be taken to avoid dependence on benzodiazepine sleeping pills. This also requires thorough education and adherence to sleep hygiene.



コメント